Wisdom teeth, also known as third molars, are the last set of molars located at the back of your mouth. These teeth typically start emerging in your late teens or early twenties, and for many people, they can be a source of discomfort and dental problems, including inflamed gums. Young adults are most commonly affected when the third molars start to emerge, and this period (often referred to as the wisdom teeth) is when problems like swollen gums and infections such as pericoronitis can develop.
In this comprehensive guide, we will explore the causes, symptoms, treatment options, and preventive measures associated with inflamed gums from wisdom teeth.
Causes of Inflamed Gums from Wisdom Teeth
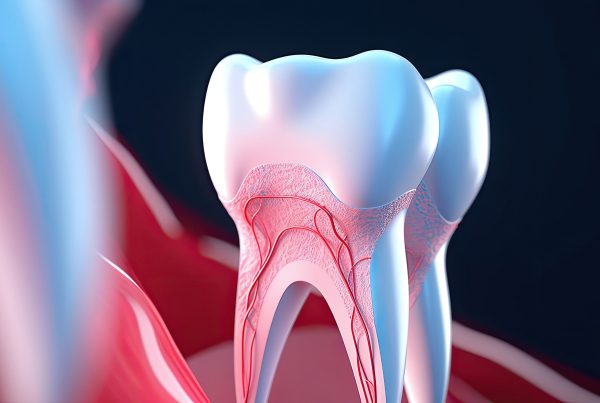
The inflammation of gums around wisdom teeth, also known as pericoronitis, is a common dental issue. Several factors contribute to the development of inflamed gums in this context, including inflammation. The gum tissue covering (a flap of gum over a partially erupted wisdom tooth) can trap bacteria underneath, leading to inflammation and increasing the risk of infection.
- Impaction: Wisdom teeth often do not have enough space to emerge properly in the mouth. They can become partially or fully impacted, meaning they don’t fully break through the gumline. This impaction creates a space where food particles and bacteria can accumulate, leading to inflammation.
- Bacterial Infection: When food debris gets trapped around partially erupted wisdom teeth, it creates a perfect breeding ground for bacteria. This bacterial infection is a primary cause of gum inflammation.
- Improper Angle: Sometimes, wisdom teeth emerge at awkward angles, pressing against other teeth or the surrounding gum tissue. This can irritate the gums, cause crowding or misalignment of other teeth, and lead to inflammation.
- Insufficient Oral Hygiene: Poor dental hygiene practices, such as infrequent brushing and flossing, can exacerbate the risk of gum inflammation around wisdom teeth. Inadequate cleaning allows bacteria to thrive and worsen the condition.
Symptoms of Inflamed Gums from Wisdom Teeth
Recognizing the common symptoms of swollen gums around wisdom teeth is important for early intervention. Recognizing the symptoms of inflamed gums around the third molar is crucial for early diagnosis and effective treatment. Common signs include:
- Pain: Persistent, throbbing pain around the back of the mouth is a hallmark symptom. The pain may radiate to the jaw, ear, or throat.
- Swelling: Swollen gums are a common symptom and can become noticeably enlarged, sometimes causing difficulty in opening the mouth fully.
- Redness: The affected gum tissue may appear red or inflamed, making it stand out from the surrounding healthy tissue.
- Tenderness: The gums may be tender to the touch, making it uncomfortable to chew or even speak.
- Bad Breath: Bacterial infection contributes to bad breath, known as halitosis, which is a common symptom of inflamed gums around wisdom teeth.
- Pus Formation: In severe cases, an abscess can form, leading to the discharge of pus from the affected area. This is a clear indication of infection.
- Facial Swelling: In severe cases, facial swelling may occur, indicating that the infection has spread and requires prompt dental attention.
- Difficulty in Opening Mouth: Extreme cases of pericoronitis can result in limited jaw movement, making it challenging to open your mouth.
- Jaw Spasms: In advanced cases, jaw spasms can develop, signaling complications that may need urgent care.
- Severe Symptoms: Symptoms that necessitate professional dental help include severe swelling, intense pain, fever, pus discharge, and difficulty swallowing.
Understanding Pericoronitis
Pericoronitis is a common gum infection that specifically affects the gum tissue surrounding a partially erupted wisdom tooth. This condition most often arises in the late teens or early twenties, a time when wisdom teeth typically start to emerge.
It is especially prevalent with lower wisdom teeth, as these are more likely to become partially erupted, leaving a flap of gum tissue—known as an operculum—over the tooth. This gum flap can easily trap food particles and bacteria, creating an environment where infection and swelling can develop. An oral surgeon or periodontist can perform wisdom tooth extraction with or without sedation to address severe cases of pericoronitis.
The presence of a partially erupted third molar increases the risk of pericoronitis, particularly if oral hygiene is not maintained. Poor oral care allows harmful bacteria and plaque to accumulate under the gum flap, leading to gum infection and, in some cases, gum disease.
As the infection progresses, individuals may experience severe pain, swollen lymph nodes, and even difficulty opening their mouth. These symptoms can escalate quickly, so recognizing early signs such as tender gums, bad breath, and bleeding gums is essential for timely treatment.
Preventing pericoronitis starts with excellent oral hygiene practices, including regular brushing, flossing, and the use of antibacterial mouthwash to remove trapped food particles and reduce inflammation.
Regular dental visits are also crucial, as a dental professional can monitor the development of wisdom teeth and recommend treatment options if impacted wisdom teeth or other issues are detected.
In some cases, a minor surgical procedure may be required to remove the gum flap or extract the infected wisdom tooth, especially if severe pain or persistent problems occur. Dentists may also prescribe antibiotics to control the infection and prevent further complications.
Additionally, using an ice pack can reduce pain and swelling in swollen gums, providing temporary relief.
Home remedies, such as rinsing with warm salt water, can help reduce pain and soothe the affected area, but professional evaluation is important to prevent the condition from worsening.
Applying a cold compress for 15-20 minutes can reduce swelling and numb pain around the wisdom tooth area.
If left untreated, pericoronitis can lead to more serious health problems, including dental abscesses and, in rare cases, life-threatening infections. By prioritizing good oral hygiene, seeking timely treatment, and maintaining regular dental check-ups, individuals can protect their overall oral health and find relief from the discomfort associated with wisdom teeth and pericoronitis.
Treatment Options for Inflamed Gums from Wisdom Teeth
The primary goal is to treat swollen gums and prevent complications associated with wisdom teeth.
The management of inflamed gums around wisdom teeth depends on the severity of the condition. Here are various treatment options:
- Oral Hygiene: Practicing good oral hygiene is crucial. Brush your teeth and gums gently with a soft-bristle toothbrush and floss daily to remove food debris and bacteria. Use an alcohol-free mouthwash to avoid further irritation.
- Warm Saltwater Rinses: Rinse your mouth with warm saltwater made by dissolving salt in warm water several times a day. This can help reduce inflammation and cleanse the area.
- Pain Relief: Over-the-counter pain relievers like ibuprofen or acetaminophen can alleviate discomfort and reduce inflammation.
- Antibiotics: In cases of bacterial infection or abscess formation, your dentist may prescribe antibiotics to clear the infection.
- Prescription Mouthwash: Your dentist may recommend a prescription mouthwash containing an antimicrobial agent to help control bacterial growth.
- Professional Cleaning: A professional cleaning by a dental hygienist can help remove bacteria and food particles contributing to swollen gums.
- Surgical Removal: If your wisdom teeth are causing recurrent or severe problems, your dentist or oral surgeon may recommend minor surgery, such as removing the gum flap (operculum) or extracting the wisdom tooth, if conservative treatments are insufficient. This surgical procedure can prevent future episodes of pericoronitis.
- Incision and Drainage: In cases of abscess formation, your dentist may need to drain the pus through a small incision to relieve pain and pressure.
- Elevating the Head: Elevating the head while sleeping can help reduce throbbing pain caused by swelling around a wisdom tooth.
Prevention Measures and Good Oral Hygiene
Preventing inflamed gums from wisdom teeth is possible with some proactive steps:
- Regular Dental Check-ups: Visit your dentist regularly for dental check-ups and X-rays to monitor the development and position of your wisdom teeth. Both upper and lower wisdom teeth, including the upper tooth, should be monitored for potential issues such as infection or misalignment.
- Proactive Extraction: If your dentist anticipates future issues with your wisdom teeth, they may recommend extraction before problems arise.
- Good Oral Hygiene: Maintain excellent oral care by brushing, flossing, and using mouthwash as recommended by your dentist.
- Saltwater Rinses: Periodically rinsing your mouth with warm saltwater can help prevent bacterial buildup.
- Dietary Choices: Choose a healthy diet rich in vitamins and minerals to maintain good oral health and prevent gum problems. Avoid sugary and starchy foods to reduce the risk of plaque formation and gum inflammation.
- Avoid Smoking: Smoking can exacerbate gum problems, so quitting or avoiding tobacco is beneficial for oral health.
In conclusion, inflamed gums from wisdom teeth, or pericoronitis, can be painful and uncomfortable. However, with proper oral care, early intervention, and, if necessary, surgical removal of impacted wisdom teeth, you can manage and prevent this condition. Wisdom tooth extraction can provide permanent relief and prevent further issues.
Regular dental check-ups are essential for monitoring the health of your wisdom teeth and preventing complications. If you experience symptoms of inflamed gums around your wisdom teeth, consult your dentist promptly to determine the best course of action for your specific situation.